Let’s face it…most of the news we are hearing these days is pretty discouraging. Runaway global climate change, poisoning of the environment, poverty, the rise of hate groups, terrorism, the takeover of democracy by transnational corporations, the possibility of a global pandemic because of antibiotic-resistant “superbugs”…the list goes on…and on…
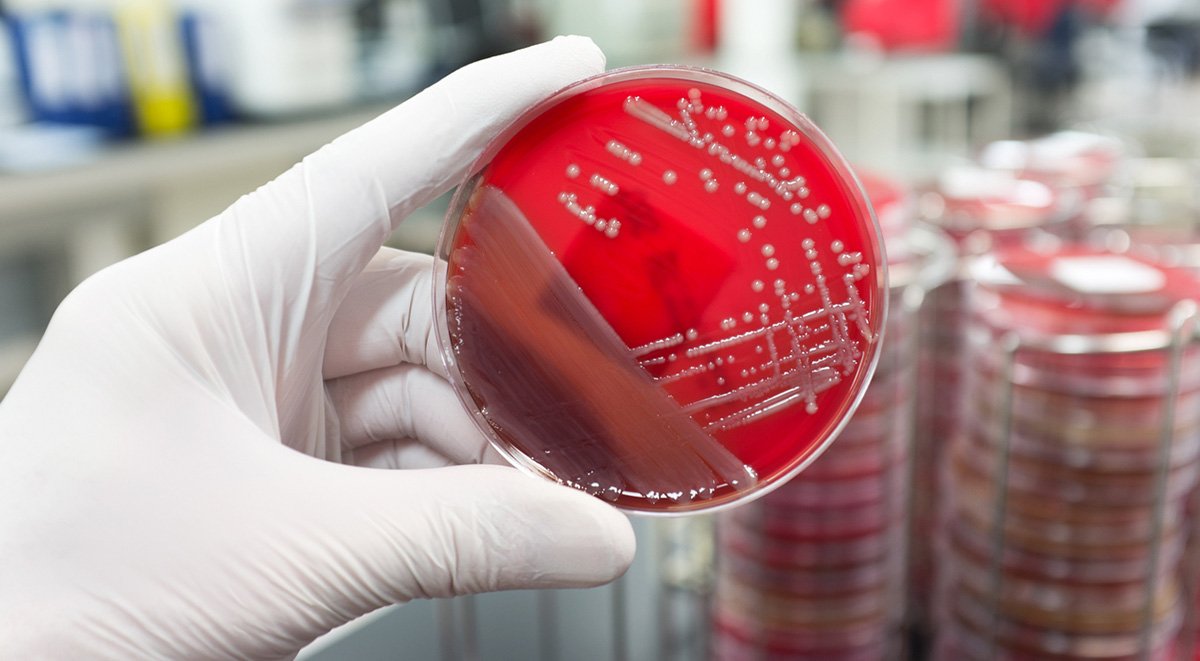
Despite all the gloom and doom however, there are reasons to be hopeful. Case in point – that last issue. The overuse and misuse of antibiotics has led to the development of drug-resistant bacteria that UN Secretary General Ban Ki-Moon describes as a “fundamental threat” to human health around the world. According to the U.K. government’s Review on Antimicrobial Resistance, such “superbugs” cause 700,000 unnecessary deaths every year – a figure that could rise to 10 million over the next three decades.
Former British Prime Minister David Cameron warned, “If we fail to act, we are looking at an almost unthinkable scenario where antibiotics no longer work and we are cast back into the dark ages of medicine.” Britain’s chief medical officer, Dame Sally Davies, described the situation as a “ticking time bomb,” placing the threat on the same level with terrorism.
That’s the bad news. Here’s the silver lining: earlier this year, researchers from Oregon State University announced the development of a molecule that actually reverses antibiotic resistance – and it is effective across numerous strains.
Lead researcher Bruce Geller points out that “We’ve lost the ability to use many of our mainstream antibiotics…everything’s resistant to them now.” One approach has been to make modifications to existing medications, but Geller points out, “As soon as you make a chemical change, the bugs mutate and now they’re resistant to the new, chemically modified antibiotic.”
The solution Geller’s team has discovered is to attack bacteria at the genetic level. The key is a specific gene, which produces an enzyme known as NDM-1. It is this biochemical substance that makes bacterial antibiotic-resistant, particularly to those in the penicillin class called carbapenems. These drugs are also the treatments of last resort. Geller explains, “The significance of NDM-1 is that it is destroys carbapenems, so doctors have had to pull out an antibiotic, colistin, that hadn’t been used in decades because it’s toxic to the kidneys…that is literally the last antibiotic that can be used on an NDM-1-expressing organism, and we now have bacteria that are completely resistant to all known antibiotics.”
The solution was to engineer a molecule that neutralizes NDM-1. The molecule is a type of “peptide-conjugated phosphorodiamidate morpholino oligomer,” or PPMO, which has a structure similar to DNA and is able to chemically bind to specific mRNA. These are messenger cells that convey genetic data from DNA to the cellular organelle known as the ribosome – which is essentially what synthesizes proteins, creating amino acid chains that are the building blocks of life itself . When those can no longer function, the bacterium is as good as dead.
It isn’t the first time scientists have attempted to employ PPMO molecules to combat antibiotic resistance. However, those PPMOs were effective only on select strains of bacteria. This new molecule targets a range of bacteria by attacking a gene common to several different strains.
“It’s the same gene in different types of bacteria, so you only have to have one PPMO that’s effective for all of them, which is different than other PPMOs that are genus specific,” Geller says.
Laboratory tests have demonstrated that PPMOs could be used in combination with existing antibiotic drugs that have been considered useless before now. The catch is that it has yet to be tested on human subjects. Clinical trials are scheduled to begin sometime within the next thirty-six months.
The study was published in the Journal of Antimicrobial Chemotherapy in December 2016.